GRACE'S BIRTH STORY:
MY MGP HOMEBIRTH
date: 6/6/2019
location: homebirth
care provider: Wollongong hospital mgp (ceri & anne)
Miro’s birth - at my home and the place where I also grew up - was the most incredible and empowering experience of my life. Pregnancy, labour and birth were an overwhelmingly positive and uncomplicated matter for me, and I think this was mainly down to three factors: knowledge, agency and support. I was lucky enough to have been born at home myself, and brought up with the narrative of pregnancy and (home) birth as safe and natural, rather than something that needs to be medicalised and feared. Before I became pregnant I knew very little about what the next 40 or so weeks would involve, so I began to do a lot of research. I read books, listened to podcasts, and asked lots of questions. This meant I started to form a strong conception of how I wanted my pregnancy and birth to progress and - just as important - what I wanted to avoid. I knew I wanted to be proactive in understanding the process and making decisions, have midwives rather than doctors, as few scans and tests as possible, and a natural intervention free birth.
With much relief I was accepted into Wollongong Hospital’s Midwifery Group Practice. My partner and I immediately fell in love with our midwife Ann and I can’t express enough how important her continuity of care was. Seeing her at every appointment allowed us to form a strong relationship where we felt complete trust, safety, comfort and support. Ann was a great source of knowledge and I never felt that I was being told what to do and how to proceed. I was not aware that you could have a home birth in the public sector so I hadn’t even imagined it as a possibility until I was four months pregnant and it was presented as an option because of renovations in the birth unit. Already aware of the benefits of home birth (both anecdotally and scientifically) I immediately said yes, and for the rest of pregnancy felt increasing excitement about, and confidence in, giving birth to my baby.
In preparing physically and mentally for birth and supporting a healthy pregnancy, I walked daily, swum regularly, practiced yoga and had lots of massage. My partner and I did a SheBirths birth course which was especially helpful in providing natural pain relief techniques, calming Michael’s growing anxiety, and imparting practical ways for him to be a supportive birth partner. I wrote a detailed birth plan and this was not only useful for my birth team, but I found it beneficial to articulate a vision of how I wanted the birth to be, and how I wanted to proceed should complications arise.
By 39 weeks we were as prepared as we could be. I’d had a few weeks off work, we’d been meeting with Ann and our second midwife Ceri at home, the birth pool was ready to be inflated, my Mum (Bronwyn) and sister (Priya) were on call to rush down from Sydney, and bub was perfectly positioned. Then I began to get lower back cramping at irregular intervals. This persisted for two days and on day three started to increase in frequency and intensity. I still went about the day - I had a long walk, cooked a hearty lunch, and did some yoga. By mid afternoon I called Michael and suggested he might want to leave work in Sydney a little early - just in case. I picked him up from the train station (by then driving was somewhat uncomfortable), and we sat down to dinner with my other Mum (Kerry) who we live with. I wasn’t able to remain sitting, however, and every so often I needed to squat/stand/stretch. I wasn’t sure if I was in labour, as I was expecting regular uterine contractions rather than irregular lower back cramps. Michael and I went for a walk to see if it would ease the discomfort, but instead every five minutes I needed to squat to ride out the increasingly intense surges. When we got home Kerry was watching the State of Origin, and whether in complete denial or deceived by my equanimity, confidently assured me I was still days away from giving birth.
By 8:30pm we thought we’d better call Ann and when she listened to me experiencing a contraction (unable to speak or answer her questions) she calmly said she’d come right over. Kerry - still in denial - called Bronwyn and Priya to let them know, reassuring them there was absolutely no rush. Fortunately they paid her no attention and got straight in the car, also paying little attention to speed limits and red lights. (Here I will note that had I been planning a hospital birth there is no way I would have been able to sit in a car for 30 minutes.)
While I had a brief shower Michael prepared the lounge-room, but by now my contractions were so frequent and intense that there was no time to inflate and fill the birth pool, put on my carefully curated playlist, or worry about aromatherapy or candles. Ann arrived at 9:15pm to find me leaning over an ottoman and suddenly and very audibly my waters broke - mostly all over Michael. At this point I was feeling a strong urge to push and the need to moan during contractions.
Bronwyn and Priya arrived, shortly followed by Ceri. Priya and Michael stayed by my side, supporting me physically and with words of encouragement. Ann unobtrusively monitored progress while Ceri took notes, Kerry assumed the mantle of photographer/videographer, and Bronwyn plied me with water and rescue remedy. It was a freezing winter night with the fire roaring, but I was boiling hot, sweating copiously and unquenchably thirsty, so the doors and windows were flung open and for the next couple of hours I drank a glass of water between every single contraction.
The intensity of sensation meant that all I could do was be entirely present and focus on breathing. I was never aware of dilation or being in transition and I couldn’t really speak or move, so mostly stayed leaning over the ottoman or in a supported stand/squat, resting in the brief moments between contractions.
Despite all my laboured pushing no progress was being made and the baby’s heartbeat began to slow. I was too focused to panic and Ann and Ceri remained unflappable, but everyone was aware there was now some urgency. Ceri then told me to redirect the energy of my vocalisations downward instead of out of my mouth, which I did to immediate effect. Within a few contractions the baby’s head was out and in the next surge, just after midnight, the body followed in one slippery gush. My physical and emotional relief was immediate and truly sublime. I held him to my chest where he coughed and spluttered and then became peaceful, our eyes staying locked for the next beautiful forty minutes. Michael was overcome, my Mums and Priya were in tears, Ann noted that bub was posterior (hence the back pain and difficulty!) and Ceri gave a rallying congratulatory speech.
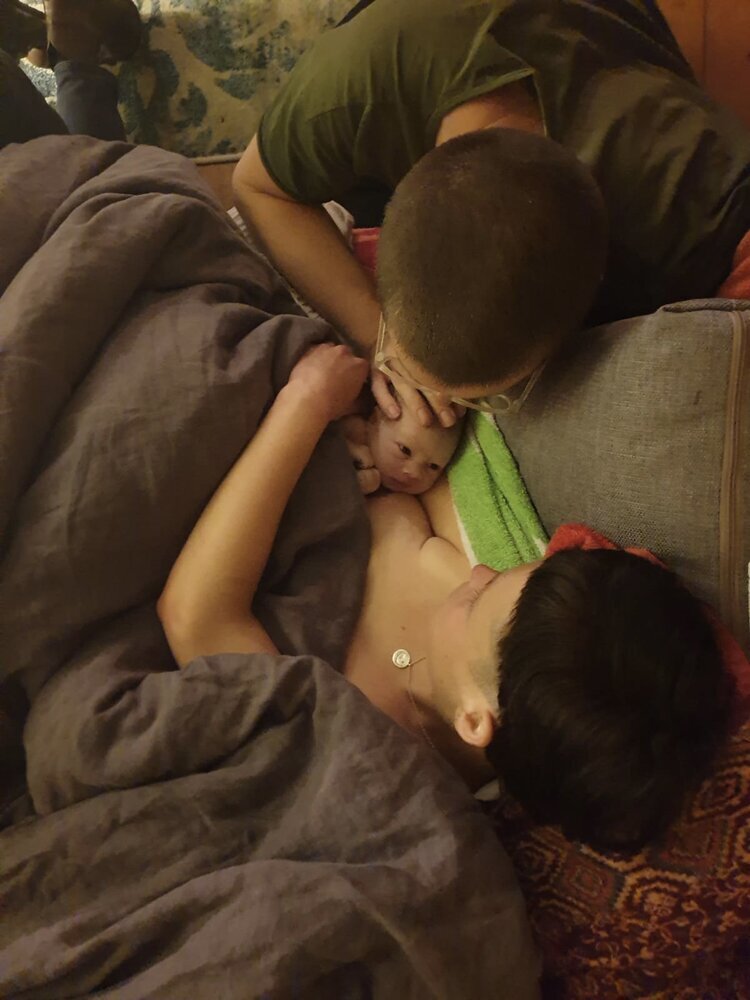
Michael cut the cord after it stopped pulsing, there was no tearing (probably thanks to perineal massage) and little blood loss. Now freezing, I was installed on the lounge with blankets and hot water bottles where the placenta slipped out around 30 minutes after birth and Miro - now named - found my breast. Michael and Miro had skin-to-skin while I had a blissful shower (and a much needed wee!), then the three of us happily went to our own bed while my family cleaned up the chaos in the lounge room.
Ann visited regularly over the next two weeks which was a wonderful support, and helped make breast-feeding problem free.
Home was the best and safest place for me to birth Miro. I felt calm, confident, strong and supported by my wonderful family and midwives, and there’s no doubt in my mind that my next baby will also be born at home.
Grace Vaughan